What’s the latest in health policy research? The Essential Scan, produced by the USC-Brookings Schaeffer Initiative for Health Policy, aims to help keep you informed on the latest research and what it means for policymakers. If you’d like to receive the biweekly Essential Scan by email, you can sign up here.
Coverage Gains among Individuals with Incomes above 400 Percent of the Federal Poverty Level Suggest the Individual Mandate Had Significant Effects
Study by: Matthew Fiedler
Though it is generally accepted that the Affordable Care Act significantly reduced the uninsured rate, the contribution to this change from the individual mandate is still debated and understanding the effect of the individual mandate is of increasing importance given the recent repeal. A new report attempts to isolate the effect of the individual mandate from other provisions (notably guaranteed issue and modified community rating).
“It is hard enough to create a viable individual insurance market with guaranteed issue and community rating with a mandate; it is substantially harder without one.” -Paul Ginsburg, Director, USC-Brookings Schaeffer Initiative for Health Policy
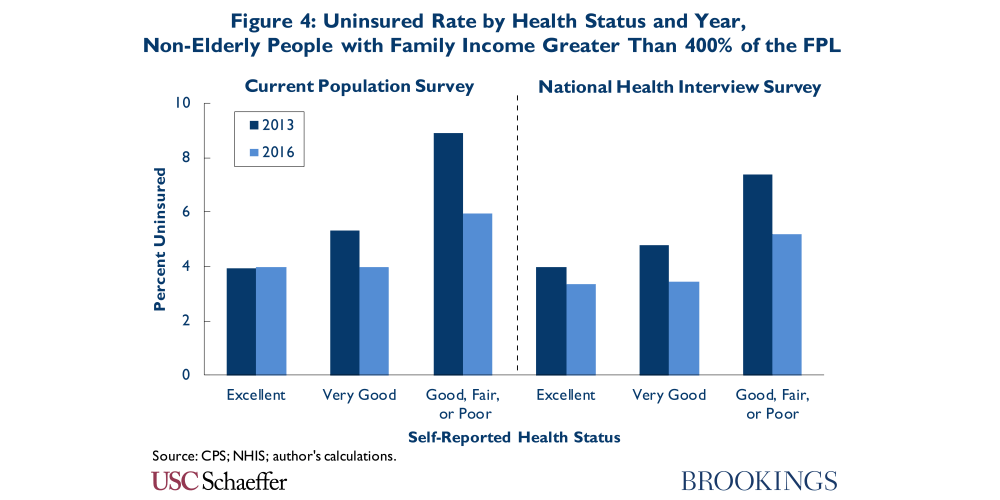
Focusing on insurance coverage trends among people with family incomes above 400 percent, who are not eligible for subsidies, the report finds the reduction in the uninsured rate among this group seems to be due in large part to the individual mandate and not the result of other provisions. For example, the uninsured rate did not meaningfully increase among healthier people in this income range, despite the fact that they typically faced higher premiums after 2013 due to guaranteed issue and community rating. “…if future state and federal policymakers wish to surpass the high-water mark for insurance coverage attained under the ACA, restoring an individual mandate or something like it should be part of the policy conversation,” wrote Fiedler in an accompanying blog post. Read the full report here and blog post here.
The Comprehensive Primary Care Initiative Improved Some Aspects of Care Delivery, But Did Not Reduce Spending Enough to Cover Management Fees
Study by: Deborah Peikes, Stacy Dale, Arkadipta Ghosh, Erin Fries Taylor, et al
In 2012 CMS launched the Comprehensive Primary Care Initiative (CPC) to test whether requiring practices to implement a new approach to delivering primary care, while providing financial and technical support, would reduce spending and improve quality over a four-year period. A new study evaluates the initiative’s effects on care delivery and outcome, comparing the 497 participating practices across the US to a set of 908 comparison practices. CPC practices reported improvements in primary care delivery and slowed growth in outpatient ED visits, relative to comparison practices. However, CPC did not reduce Medicare hospitalizations or Parts A and B spending enough to cover care management fees. Furthermore, the researchers found the only appreciable improvement in patient experience was more follow-up care after hospitalizations and ED visits. As payers move toward adopting alternative payment models that reward quality and value, “CPC provides important lessons about supportive practices in transforming care,” conclude the authors. Full study here.
Odds of Being a Frequent Emergency Department User Lower Post- ACA for Medicaid Patients
Study by: Shannon McConville, Maria C. Raven, Sarah H. Sabbagh, and Renee Y. Hsia
Policymakers hoped that by expanding health insurance coverage through the Affordable Care Act (ACA), frequent emergency department (ED) use would decline. A new study uses data from California’s Office of Statewide Health Planning and Development to compare the characteristics of frequent ED users (defined as patients with four or more annual ED visits) among nonelderly adults in California before and after implementation of several major expansions of the ACA. Researchers found that there was a 7.6 percent increase in the share of frequent users post-implementation. However, after controlling for factors such as health status, primary insurance coverage source, and county of residence, the authors found that ED patients actually had a lower likelihood of being frequent users following ACA implementation. They concluded that expanded Medicaid coverage might have allowed patients to access necessary medical services outside of the ED, but acknowledged that there has been an overall increase in both the share and the absolute number of frequent ED users. Frequent ED use has long been targeted as an area for potential cost-reduction initiatives, but this study suggests that insurance coverage alone is likely not enough to reduce overall ED visits. Full study here.









Commentary
The essential scan: Top findings in health policy research
June 7, 2018